- 05/02/2017
- Dr. Srivatsan Gurumurthy
- 0 Comments
- Blog
Facts about the Frustrating Fistula
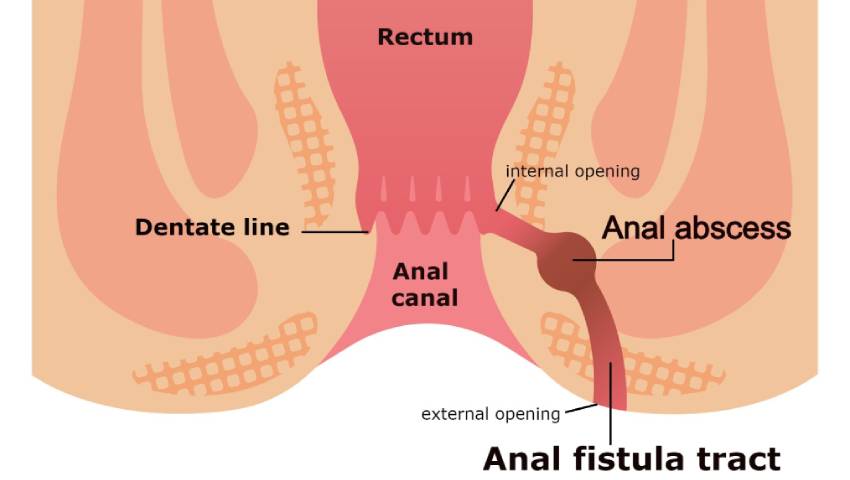
Anal Fistula (Fistula in Ano) is an abnormal passage or a track (communication) between the interior of the anal canal or rectum and the skin surface. Rarer forms may communicate with the vagina or other pelvic structures, including the bowel, says Consultant Gastroenterologist, Dr S Srivatsan Gurumurthy
Historical connotation:
The disease -anal fistula is as old as mankind. Thousands of years ago, Hippocrates made reference to surgical therapy for fistulose disease. English surgeon John Arderne (1307-1390) wrote “Treatises of Fistula in Ano; Haemorrhoids, and Clysters” in 1376, which described fistulotomy and the use of seton suture for the same.
Textual and contextual evidence suggests that the French king’s fistula, a central plot device in Shakespeare’s play All’s Well That Ends Well, is a fistula-in-ano. Anal fistula was known to the lay public in Shakespeare’s time. In addition, Shakespeare may have known of the anal fistula treatise of John Arderne, an ancestor on Shakespeare’s mother’s side. All’s Wed That Ends Well tells the story of a physician’s daughter, Helen, who succeeds in curing the French King of his debilitating fistula.
No passage in the play gives any clue as to the exact site or nature of fistula. One is left to surmise that it could be the common fistula-in-ano, about which John of Arderne — the Father of Proctology — wrote extensively; it could alternatively imply a chronic abscess with discharging sinus, involving the finger or breast.
Historical references indicate that Louis XIV was treated for an anal fistula in the 18th century. In the late 19th and early 20th centuries, prominent physician/surgeons, such as Goodsall and Miles, Milligan and Morgan, Thompson, and Lockhart-Mummery, made substantial contributions to the treatment of anal fistula. These physicians offered theories on pathogenesis and classification systems for fistula-in-ano.
Over the last 50 years many surgeons have presented new techniques in an effort to minimise recurrence rates and incontinence (loss of control over passing stools) complications. But despite 2500 years of experience, anal fistula remains a perplexing surgical disease.
The Course Of Events:
There is a relation between a perianal abscess and a fistula in ano: almost always a fistula develops as a result of an abscess. When the abscess opens spontaneously (or has been opened surgically), a fistula may occur. An anal abscess is an infected cavity filled with pus found near the anus (the opening of the anal canal) or rectum (the portion of large intestine just proximal to the anal canal).
This can result from a blockage of the anal glands located just inside the anus. An abscess produces pain and swelling near the anal opening. Fever may also be present. If left untreated, the abscess can “bore” through internal tissues – thus creating an unnatural “tunnel” which may or may not have a painful external opening. This tunnel, called fistula or fistula-in-ano can have several branches.
Fistula can develop from an untreated abscess inside of the anal canal, and can also be a symptom of a digestive ailment called Crohn’s disease belonging to a group of disorders called inflammatory bowel diseases. Other factors that may create or exacerbate fistula are: HIV infection, tuberculosis, and radiation therapy for prostate or rectal cancer. Fistulas may occur singly or in multiples.
Common Complaints:
The first signs of fistula are a throbbing sensation, visible opening, swelling, and tenderness. Often, foul-smelling pus from the infected glands seeps out from the fistula. In rare cases, feces can also pour out of the fistula during bowel movement.Fistula in ano generally presents as a small boil – like opening around the anus at a distance of few mm. to a couple of inches, in any direction. Pus or blood keeps on oozing out of this opening, continuously.
Patients often give a history of previous pain, swelling, and spontaneous or planned surgical drainage of an anorectal abscess.
Perianal discharge, painful swelling in the perianal region, bleeding, skin excoriation and a visible external opening in the perianal region.
A physician may be able to diagnose an anal fistula by physically examining the area surrounding the anus. However, if external signs, such as an opening in the skin, are missing, then an internal exam will be necessary. An instrument called a proctoscope is used to inspect the anal canal.
Radiological Investigations:
These are not performed for routine fistula evaluation. They can be helpful when the primary opening is difficult to identify or in the case of recurrent or multiple fistulae to identify secondary tracts or missed primary openings.
- Fistulography: This involves injection of contrast via the external opening, which is followed by x-ray images to outline the course of the fistula tract.
- MRI: Findings show 80-90% concordance with operative findings when observing a primary tract course and secondary extensions.
Treatment Options:
- Surgery- Fistulotomy/fistulectomy: An anal fistula usually lasts until it is surgically removed. The fistula tract must be opened along with the source of the infection. Usually, tissue around the external opening and the internal opening is excised along with a small margin of tissue lining the tract, called a fistulotomy. Excision of the complete tract is called a fistulectomy. The laying-open technique (fistulotomy) is useful for 85-95% of primary fistulae. Complete fistulectomy creates larger wounds that take longer to heal and offers no recurrence advantage over fistulotomy.
- Seton placement: Fistulotomies work well for fistulas that are relatively close to the skin. For deeper fistulas, however, the surgeon may choose to use a seton. A seton is a piece of suture material that is passed from the external skin opening, along the fistula tract, through the internal opening in the anal canal, exiting through the anus. The suture material is then tied in a loop, which is gradually tightened over a period of weeks. This ultimately has the same effect as a fistulotomy—to open the fistula tract and allow it to heal.
A seton ( thread tie ) can be placed alone, combined with fistulotomy, or in a staged fashion. This technique is useful in patients with the following conditions:
- Complex fistulae
- Recurrent fistulae after the previous fistulotomy
With time, healing occurs above the seton as it gradually cuts through the muscles. The seton is tightened on subsequent weekly visits until it falls out. This could take 2-5 visits to cure.
After either fistulotomy or fistulectomy there is an open wound left which is packed for a few days. Nursing care is required for a varied period of time which depends on the size of the wound and the degree of associated infection. At some point, dressings stop being necessary and the patient can continue the treatment with sitz baths. Life with a fistula can be normal if sepsis or infection is avoided. Hot salt baths (sitz bath) help to soothe and irrigate the area minimising infection.
Recurrence is common with fistula surgeries.This is because, as explained above, infections in this area are difficult to eradicate and surgery is limited by the risk of incontinence. Incontinence (loss of control over passing stools) is associated with a high anal fistula type of surgery and previous fistula surgery.
There is a direct relationship between incontinence and the amount of sphincter muscle divided. The goal of surgical treatment is thus two-fold- to eradicate the suppurative process permanently without compromising anal continence.